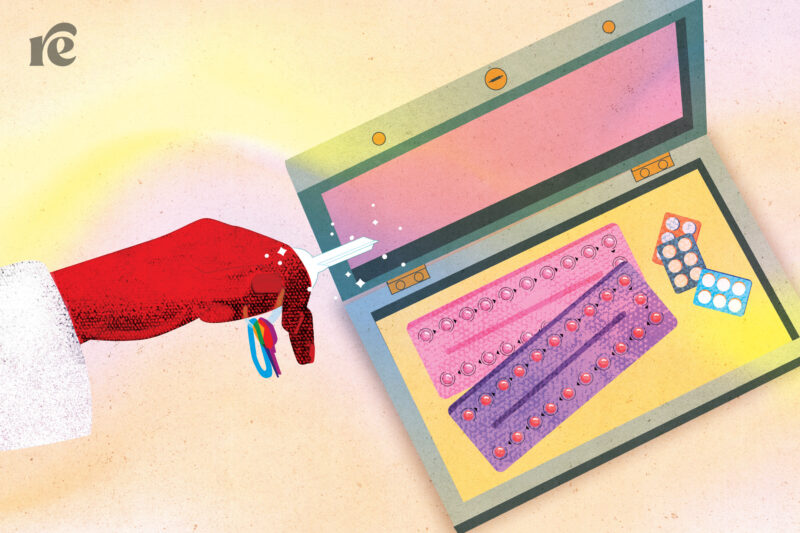
A Birth Control Pill Could Be Available Over the Counter for the First Time
Here’s what you need to know about the historic FDA hearings on over-the-counter birth control access.
Update, May 11: On May 10, joint FDA advisory committees voted unanimously to recommend that the FDA make Opill available over the counter. A final decision is expected from the FDA this summer.
Did you know that in over 100 countries around the world, you can walk into a pharmacy and buy birth control pills without a prescription?
The United States is not one of those countries.
In fact, the United States and Western Europe are woefully behind the times on this front: In most other regions of the world, at least some contraceptive pills are broadly accessible over the counter (OTC). But we might finally be catching up: On May 9 and 10, a Food and Drug Administration committee will hold hearings that could result in a birth control pill called Opill becoming available over the counter. If approved, Opill will be the first OTC contraceptive pill in the United States.
May 9 also happens to be Free the Pill Day, the anniversary of the FDA’s first approval of a birth control pill in 1960. Sixty-three years later, the agency has an opportunity to make history again. Making birth control available without a prescription would be groundbreaking no matter what, but the decision is especially consequential at this moment given the conservative push to turn the clock back to the 1950s—or even the 1870s.
Here’s the background you need to understand what’s going on.
What’s happening with Opill
Opill is already an FDA-approved drug. In fact, its active ingredient has been approved since 1973. Just like any other birth control pill, you can get it by prescription from a health-care provider. However, in order for an approved drug to become available OTC, it has to go through another review process.
In that process, the drugmaker has to prove a few things:
- That people can understand how to use the drug;
- Determine whether or not the medication is appropriate for them without consulting a medical provider;
- Take it as directed;
- And do all of that based on the information provided on the label.
Once a pharmaceutical company has submitted the necessary research proving these points, the FDA conducts an internal review. Sometimes they seek input from an advisory committee, which makes a recommendation after hearing testimony from experts and members of the public. That’s what next week’s hearings are for.
The hearings were originally scheduled for late 2022, but were abruptly postponed. The FDA typically aims to finish reviewing these types of applications within ten months of when they’re submitted, and we’re nearing that ten-month mark now.
Why hasn’t this happened before?
According to the Centers for Disease Control and Prevention, a whopping 82 percent of sexually active women in the United States have used the birth control pill at some point. The American College of Obstetricians and Gynecologists, American Academy of Family Physicians, and American Medical Association all support OTC hormonal contraceptives.
So why has it taken us so long to get here?
Well, contrary to the common idea that birth control is a Big Pharma conspiracy motivated by profit, pharmaceutical companies aren’t particularly interested in birth control pills. That’s because, compared to a lot of other medications—especially newly developed drugs still under patent that retail for astronomical prices—birth control is cheap. Pharmaceutical companies don’t see a big potential for profit there even though so many people use them. For most pharma companies, the status quo—where millions of people get the pill by prescription—has been working just fine.
There’s also the unavoidable fact that anything having to do with sex—especially young, unmarried people having sex—is something that conservatives will turn into a controversy.
Back in 2011, for example, then-Secretary of Health and Human Services Kathleen Sebelius took the unusual step of reversing the FDA’s decision to bring one of the forms of emergency contraception, Plan B, over the counter for all ages. (Though Plan B works similarly to birth control pills, it’s taken one time after sexual activity to prevent pregnancy rather than on a regular basis.) President Barack Obama supported the decision publicly, expressing concern about teens using Plan B in a way that many people saw as paternalistic. Plan B didn’t become available OTC for all ages until 2013, and even then it was only because of a judge’s order.
Opill is a progestin-only pill. Here’s what that means.
Most people who have taken hormonal contraceptives have taken a combined oral contraceptive pill, or COC. This type of pill contains synthetic versions of two hormones, estrogen and progesterone (which, in its synthetic form, is called progestin). But there’s another type: the progestin-only pill, or POP. You might have heard this called the “mini-pill.”
While fewer people are familiar with POPs, they have a lot of benefits. For one, while all birth control pills are very safe overall, estrogen-containing pills can increase the risk of blood clots and stroke in some people, especially those already predisposed to such conditions. This risk is much lower than it used to be, because modern birth control pills contain far lower hormone doses than older versions. However, because POPs contain no estrogen, they don’t carry this risk at all. That means they’re appropriate for a broader group of people, making them a great OTC test case.
If you are familiar with POPs, you might have heard that they must be taken at exactly the same time each day—down to just a three-hour window—in order to work properly. But there are different forms of progestin that work to prevent pregnancy in slightly different ways, and newer research finds that not all of them require quite such a strict schedule. Great news: Norgestrel, the progestin that’s in Opill, is one of these. In other words, like any birth control pill, users should strive to take the pill at the same time each day. But with Opill, you’ve got a little more wiggle room than three hours.
The conventional wisdom used to be that POPs were slightly less effective than COCs, but updated research is challenging that, too. With perfect use—meaning you take the pill at exactly the same time every day—POPs are 99 percent effective. With typical use, they’re 93 percent effective, same as COCs.
Benefits of over-the-counter access
It’s not easy for everyone to get the pill by prescription: In 2015, a study found that more than one-third of adults who had ever gotten a prescription or refill for a birth control pill faced some sort of barrier. In a more recent study looking at the experiences of Black, Indigenous, and people of color, nearly half of participants reported facing a roadblock of some kind.
Another group that stands to benefit from OTC birth control? Teens, who might want to keep their birth control use private or who may have trouble getting to the doctor because they’re reliant on others to get them there, to name a few potential challenges.
While bringing the pill over the counter will eliminate the need to go to the doctor to get a prescription, it may or may not address another major limiting factor: cost. That’s why advocates are calling on the federal government to require insurers to cover OTC contraceptives without a prescription, and on pharmacies and pharmaceutical companies to keep costs low in general.
What happens next
After the hearings on May 9 and 10, the FDA will issue a decision whenever it wants. I’ll be live tweeting the FDA hearings, so be sure to follow Rewire News Group on Twitter to stay up to date.
