The Ban on Federal Funding for Needle Exchanges Puts Poor Women in Danger
Thanks to restrictive laws and limited health-care options, halting the spread of HIV and hepatitis C is often a losing battle—one that puts women substance users in particularly high danger.
Intravenous drug use has surged in the United States over the last decade. Though media narratives around the uptick tend to focus on crime rates or overdose, the risk of contracting HIV or hepatitis C through used needles is also a major public health concern. And thanks to restrictive laws and limited health-care options, halting the spread of these infections is often a losing battle—one that puts poor women in particularly high danger. Yet Congress still refuses to provide the federal funding that could be key to combating this crisis.
Many intravenous substance users are at heightened risk of contracting HIV or hepatitis C from sex work or sexual violence. According to a 2010 study by the Reference Group to the United Nations on HIV and Injecting Drug Use, between 15 and 66 percent who use injection drugs engage in sex work. Daniel Raymond, the policy director at the Oakland, California-based Harm Reduction Coalition, noted that clients often offer to pay sex workers more for unprotected sex. He also added that in some places, law enforcement can point to condoms as evidence of prostitution, which discourages sex workers from carrying them.
The UN report also stated that women who use intravenous drugs are subjected to higher levels of violence, including sexual abuse. Among other mental, emotional, and physical consequences, these assaults can also lead to sexually transmitted infections.
For poor or homeless women with HIV or hepatitis C, accessing care options at all can be nearly impossible. In some states—California, for example—Medicaid doesn’t cover hepatitis C treatments unless a patient has very advanced liver disease and can prove either six months of substance abstinence or is in a treatment program.
And if those women become pregnant, that can lead to serious ramifications for their children, too. Pregnant women with untreated HIV have a 25 percent chance of passing the virus on to their babies during gestation or delivery. Meanwhile, according to Emalie Huriaux, the director of federal and state affairs at the San Francisco-based advocacy group Project Inform, only about 5 percent of women with hepatitis C transmit the virus to their baby—but infants who do contract it are at risk for developing cirrhosis or liver cancer as adults. This is not to mention the hardships that come from trying to raise an infant as a parent with an expensive, often debilitating disease.
In order to combat this cycle of complications, many grant-funded centers across the country provide free resources that promote healthy living for women, including condoms and other contraceptives, referrals to prenatal care, and lists of people potentially dangerous to sex workers. Many also offer treatment for HIV and hepatitis C; the former can help drive down a pregnant woman’s viral load before birth and protect babies from infection during breastfeeding, and the latter can help women keep from spreading the infection further. Additionally, evidence shows that even when infections are not a factor, prenatal care can reduce the effects of substance use on perinatal outcomes.
Unfortunately, care providers say, drug users are often met with suspicion or even punishment when they need medical care. As a result, they are often hesitant to seek out help when they need reproductive services.
“There’s such a tremendous amount of stigma within the health care system around people who use drugs,” said Whitney O’Neill Englander, government relations manager for the Harm Reduction Coalition. “And women who use who have children or are pregnant have the highest amount. You see it play out in people taking women’s children away from them based on no evidence they’ve harmed them. You hear a lot about people calling child protective services if there are children involved. It’s pretty routine in terms of if a mother says she has used drugs while pregnant.”
This understandable fear of going to the doctor, or being honest about their drug use if they do go, puts mothers’ health—and the well-being of their fetuses, children, and communities—in further jeopardy.
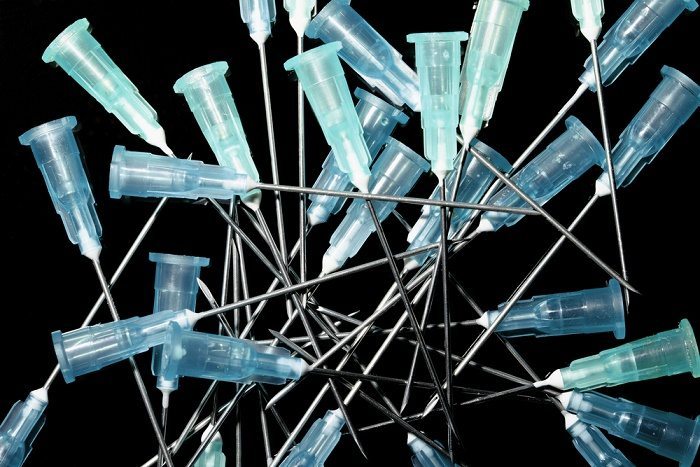
One way to overcome this reluctance among substance users, advocates say, is to combine reproductive health care with needle exchanges, which provide individuals with sterilized syringes in exchange for ones that could be contaminated.
“Needle exchanges are among the only way to get women who are at high risk in the door,” Mary Wheeler, outreach program director at Randolph, Massachusetts-based Healthy Streets, told Rewire. “When you’re using, you need needles on a daily basis. Syringe exchange programs get more people involved in health-care treatment.”
Needle exchange programs, which became popular in the 1980s, have proved to be key in driving down HIV and hepatitis C infection rates; they also offer counseling services to users trying to curb the habit. Unfortunately, the practice has regularly faced controversy from both law enforcement and policy-makers. In many states, the vague wording around exchange legality can leave advocates vulnerable to arrest. The Obama administration lifted a ban on federal funding for exchange programs in 2009; in 2011, Republicans in Congress reinstated it. As of now, there are only 227 reported programs total in the United States.
Many groups around the country, such as Wheeler’s Healthy Streets, use their syringe exchange programs to connect users to other health services like prenatal care. They label themselves as “harm reduction organizations,” meaning that in addition to such referrals, they prioritize giving drug users and sex workers tools to keep them safe, such as clean needles, filters, and antiseptic towelettes. This positions them as a partner in preserving women’s health, advocates say, rather than a foe.
“Syringe exchange programs are vital for these women in order to have an ally who has the mother’s best interest in mind,” said Catherine Paquette, mobile services manager at the Washington, D.C., harm reduction service HIPS.
Harm reduction as an approach is controversial because many legislators and members of the public make the knee-jerk assumption that it signifies approval of drug use. But it’s worth stating clearly that syringe exchange programs are not federally illegal; they just can’t be paid for by federal dollars. Aside from keeping programs from using money they’re already receiving (for HIV testing from the Centers for Disease Control and Prevention, for instance) that limitation also bottlenecks funds that could be coming from state and local sources.
“States are not undertaking syringe programs because they see the federal ban as sort of a scarlet letter,” Michael Collins, policy manager at the Drug Policy Alliance, told Rewire. “When the ban was lifted during the Obama administration’s first two years, we did see an uptick in states’ interest and funding. When we have the ban in place, it’s incredibly counterproductive for states having syringe programs.”
In Massachusetts, for instance, only ten syringe exchange programs can receive funding from the state’s health department, and each needs approval from its respective local government. Wheeler’s organization, Healthy Streets, is limited to running a voucher program that routes clients to pharmacies where they can receive clean needles because the city Randolph doesn’t allow exchange programs.
“I think people are still unwilling to look at substance use as a public health issue,” said Wheeler. “People are scared of folks who inject drugs. The idea in Massachusetts is still pretty strong that if you have a needle exchange in your community, drug use and crime increases, despite all the evidence that that’s not true.”
Meanwhile, in Washington, D.C., Paquette’s organization, HIPS, started its syringe exchange program in 2007 after Congress lifted a rider that kept the district from funding the group. Using money from the D.C. Health Department, the MAC AIDS FUND, and the Syringe Access Fund, the group’s syringe exchange program reaches not only intravenous drug users but also transgender women who use needles to inject hormones. It also provides ancillary supplies that make injecting safer, like cookers and cotton swabs.
Since D.C. first allowed needle exchanges, there’s been an 80 percent drop in HIV rates among drug users. Still, HIPS could do more if the federal funding ban was not in place, like apply for federal grants to expand and enrich syringe exchange programming. Also, employees whose salary is even partially supported by one of the CDC grants that funds HIPS’ HIV prevention services cannot help with the organization’s syringe exchange branch. In practical terms, that means that while certain HIPS workers can administer an HIV test, lead a support group, or hand out condoms to clients, they have to stop what they’re doing and go get a colleague if those same clients want trade dirty needles for clean ones.
“It’s an administrative annoyance,” said HIPS Executive Director Cyndee Clay. “It takes up time and resources that without the federal ban we wouldn’t have to worry about. The CDC is all about high-impact prevention but can’t talk syringe exchanges. It’s just silly.”
It doesn’t look like the ban will be lifted any time soon, particularly now that Congress is wholly under Republican control. Because it needed compromise on a number of controversial issues in order to reach an agreement in final negotiations, Congress passed the 2014 budget as an omnibus appropriations bill. And since the exchange funding ban is packaged alongside the Affordable Care Act and a number of abortion laws in the Departments of Labor, Health and Human Services, and Education appropriations bill, Democrats did not make rescinding it a priority.
Advocates anticipate that rolling back the ban would require a focus on the issue that many Democrats may not be willing to give. Among many Republicans, Collins says, syringe exchange funding is frequently conflated with government support for drug use.
“The nuances of harm reduction and what harm reduction is not are often present in those offices,” said Collins. “There are a number of Republicans in positions of power, mainly Hal Rogers, who want this ban to remain in place, and I think part of it is a belief that states and local authorities can fund this out of their own pocket, and part is this misguided notion that syringe programs encourage heroin use.”
In reality, harm reduction through syringe exchange benefits the general public as well as injection drug users. In August 2013, then Seattle police chief Jim Pugel wrote a well-circulated op-ed calling Washington “healthier and safer” thanks to the state’s exchange programs.
Syringe exchange programs also save taxpayers money because the costs of HIV and hepatitis C prevention are far less than the costs of treatment: A CDC study found the average cost of a prevented HIV infection by way of a syringe exchange program to be between $4,000 and $12,000. The cost to treat a person infected with HIV? $190,000. With the cure for hepatitis C being marketed at $1,000 per pill, or $80,000 total, the cost comparison is similar. This is not to mention the indirect benefits that come from connecting users with preventive care, including reproductive services.
Perhaps the best reason to re-examine the federal ban on needle exchange funding, however, is to remember the death toll caused by the diseases that exchanges help fight. According to AVERT, an international AIDS and HIV charity, 2011 saw more than 20,000 AIDS-related deaths in children and adults in North America; the CDC reports that hepatitis claims the lives of up to 15,000 people in the United States annually. Given what we know about syringe exchange programs, Congress could be doing more to curb these numbers.
“I work for a number of different issues and this is probably the most frustrating because it’s the most common-sense policy,” said Englander. “You save lives, connect people to treatment, have support of law enforcement. It’s really not acceptable that it’s not utilized because of political reasons. We’re breeding a very expensive health problem.”

