Women of Color More Likely to Give Birth in Hospitals Where Catholic Beliefs Hinder Care
Women of color bear the brunt of Catholic hospital restrictions on abortion, sterilization, contraception, gender-affirming procedures, and other care under religious directives.
When Laurie Bertram Roberts was 12 weeks pregnant, she noticed a pink discharge running down her leg. She went to her local Catholic hospital in Indiana. They sent her home and told her to come back if she started bleeding. After she began bleeding heavily the next day, she returned to the hospital, where providers confirmed Bertram Roberts was miscarrying and her pregnancy was not viable.
But because the fetus still had a faint heartbeat, they said they couldn’t do anything to help her. Instead, they sent Bertram Roberts home again.
Hours later, Bertram Roberts passed what she believed was her pregnancy into the toilet. She was bleeding so heavily that she put on a child’s diaper. Then she blacked out, Bertram Roberts told Rewire in an interview. She felt like she was going to die. One of the paramedics, her neighbor, was uncharacteristically serious, which scared her. She felt cold, which she realizes now was likely her body going into shock.
After she arrived at the hospital, she remembers hearing her doctor yell, “Who the fuck sent her home? She could have died!”
Catholic hospitals restrict access to abortion, sterilization, contraception, gender-affirming procedures, and other care under religious directives, which govern one in six acute-care beds nationwide.
A groundbreaking report reveals how women of color like Bertram Roberts bear the brunt of these restrictions. Researchers with Columbia Law School’s Public Rights/Private Conscience Project analyzed data from 33 states and Puerto Rico. In 19 of those states, women of color were more likely than white women to give birth at a Catholic hospital. Nationally, 53 percent of births at Catholic hospitals are to women of color, versus 49 percent of births at non-Catholic hospitals.
“Pregnant women of color are more likely than their white counterparts to receive reproductive health care dictated by bishops rather than medical doctors,” the authors wrote in the report, “Bearing Faith: The Limits of Catholic Health Care for Women of Color.”
The results are particularly stark in some states:
- In New Jersey, women of color represent 80 percent of births at Catholic hospitals, even though they make up only half of all women of reproductive age, and 53 percent of births at non-Catholic hospitals.
- In Maryland, three quarters of births at Catholic hospitals are to women of color, who make up less than half of births at non-Catholic hospitals. While Black women in Maryland had 10,000 fewer births overall, they had nearly 3,000 more births at Catholic hospitals than white women.
- In Maine, Black women are nearly three times more likely than white women to give birth at a hospital that follows Catholic restrictions.
- In Wisconsin, which was the setting of a Rewire investigation about a doctor who was forced to watch her patient sicken at a Catholic hospital, more than half of births to Black women take place in Catholic hospitals, versus one in three births to white women.
The Trump administration on Thursday moved to give these hospitals broader latitude to deny care to patients, unveiling a new Conscience and Religious Freedom Division to protect providers who reject transgender patients or refuse to perform medical procedures like abortions.
“This office is giving providers a license to discriminate,” Susan Berke Fogel, director of reproductive health at the National Health Law Program told Rewire. “The government is going to give these providers permission to deliver substandard care.”
And as the new report shows, these restrictions won’t fall equally on all patients.
“Whenever there is any type of law or guidelines that can cause harm, I think that people need to take the necessary look at how those type of laws harm those who are the most disenfranchised and the most vulnerable, and those are usually women and people of color,” Kira Shepherd, co-author of the “Bearing Faith” report, told Rewire in an interview, before the new office was announced.
“Even Serena Williams … Has to Fight”
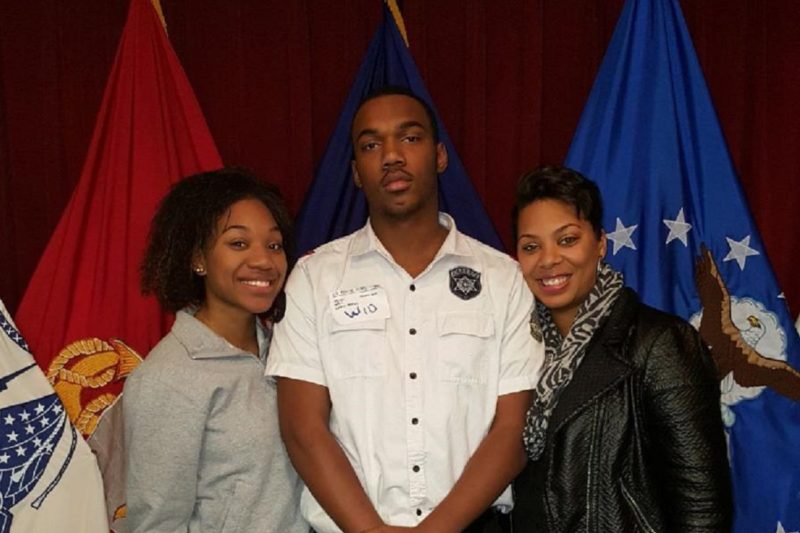
Bethany S. Watkins knew what she wanted.
After delivering her second child in 2000, Watkins asked her doctor for a tubal ligation. But her doctor wanted her to wait. So Watkins went home, prayed about it, and still, she felt certain; she was satisfied with her two children. But when she went back to her doctor, he told her he couldn’t perform the surgery because the Hospital of Saint Raphael, in New Haven, Connecticut, where he operated, “will not accept your case.” He said the hospital would reject her because she was only 22.
“Both of my children were born at Saint Raphael’s,” Watkins told Rewire in an interview. “So it was OK for me to give birth as a young, unwed mother but it wasn’t OK for me to take control of this happening again.”
In Connecticut, the report found, women of color like Watkins are more than twice as likely as white women to give birth in a Catholic facility.
Watkins didn’t give up. Two other doctors turned her down before she finally found one who would perform the surgery. She’s never regretted it.
Watkins had never considered that religion may have played a role in her saga. But in October, as she watched a presentation by Shepherd at a summit hosted by the reproductive justice group SisterReach, Watkins almost fell out of her chair.
Shepherd talked about how Catholic hospitals restrict access to care, including tubal ligations. “I was like, oh my God, that’s why they wouldn’t do it,” Watkins said.
It’s unclear how much of a role religion played in her denial. Catholic hospitals often ban or heavily restrict tubal ligations under the Catholic directives, but it can be difficult for young women to obtain sterilizations even without these rules. Yale-New Haven Hospital, which acquired Saint Raphael in 2012, said the campus “is not a ‘Catholic hospital'” but operates under a commitment “to provide medical care in a manner that supports the intent of the [directives] and is consistent with prior practice on that campus.” A spokesperson did not immediately respond to follow up questions about exactly what that means.
For Watkins, who said she had to cajole a doctor into performing a hysterectomy on her in 2016 after she suffered for years from painful fibroids, it was yet another time when, as a Black woman, she had to fight for what she needed.
“I always feel like I have to fight,” Watkins said. “I always feel like I have to prove my worth. I have to prove that I have two kids that are doing well; I can make good decisions. ‘See? I’m competent, I’m smart, I’m intelligent, and here’s my family history—please, please, please?’ Why can’t I just walk in and say, ‘medically, I qualify?’”
Discrimination against Black women in medicine has become a topic of national conversation. Black women are 243 percent more likely than white women to die from pregnancy or childbirth-related causes. Tennis great Serena Williams called attention to this disparity when she shared her story of having to walk providers through saving her life when she developed a pulmonary embolism after giving birth.
“Even Serena Williams … she’s iconic, and she still has to fight,” Watkins said. “So who the hell am I?”
10,000 Fewer Tubal Ligations Across the U.S.
One of the best-known cases of denial by a Catholic hospital is that of Tamesha Means, a Black woman who was sent home twice by Mercy Health Partners in Muskegon, Michigan, in 2010 after her water broke when she was 18 weeks pregnant. The American Civil Liberties Union (ACLU) filed a lawsuit on her behalf, which was dismissed. Brigitte Amiri, ACLU senior staff attorney, said the new report raises questions about future legal strategies, such as whether claims could be brought under racial discrimination statutes.
Faith Groesbeck, who blew the whistle on denials of care at Mercy Health Partners after working as a public health researcher for Muskegon County, said racial bias can compound religious restrictions. The Catholic directives are subject to interpretation, from the local bishop, the hospital, and even the doctor.
“I saw, for example, a white woman come in who was in early labor, and in danger of miscarriage, and the provider created a loophole so she could get transferred to another hospital where the provider would not be limited in her care options,” Groesbeck said. “But people are more likely to create those loopholes when they empathize with the patient, and they’re more likely to empathize with a patient that reminds them of themselves.”
On top of that, Black women are at a higher risk of having their water break before fetal viability, resulting in the kinds of denials Means experienced.
Yet patients like Watkins remain largely unaware of these restrictions.
In a recent survey, about a third of women of reproductive age said it was somewhat or very important to know a hospital’s religion—but that number increased to 80 percent when researchers asked how important it was to know about restrictions on care. To survey co-author Lori Freedman, that shows many patients are unaware of how religious hospitals may deny access to services.
“Potential patients aren’t thinking ahead of time: Well, I need to find out what reproductive services are restricted or not before I go seek help during a miscarriage or before I decide where to deliver my baby and want a sterilization,” Freedman, a professor at the University of California San Francisco, told Rewire.
From 2001 to 2016, the number of acute-care hospitals that are Catholic owned or affiliated increased by 22 percent, despite an overall drop in the number of such hospitals. Forty percent of the largest health-care systems were faith-based as of 2016. The impact has been dramatic: a recent study found that Catholic hospitals reduce the per-bed annual rates of inpatient abortions by 30 percent, and tubal ligations by 31 percent. That amounts to about 10,000 fewer tubal ligations annually across the United States, the researchers found.
These trends disturb Laurie Bertram Roberts, co-founder and executive director of the Mississippi Reproductive Freedom Fund, when she reflects on her experience with the Catholic hospital as a teenager.
“This was 22 years ago, and it’s not better for women like me, it’s worse,” she said. “To me [Catholic hospitals] can’t even make the case that they’re not sacrificing safety. There is no medical argument for what they are doing …. This is purely their religious beliefs being forced upon unwitting, unknowing patients. How dare they?”
The reasons why women of color disproportionately give birth in Catholic hospitals remain elusive. But it’s not because Catholic hospitals provide more charity care than other hospitals. As the report notes, they do not.
To raise awareness of these restrictions among potential patients requires a “ground strategy,” said Cherisse Scott, founder and CEO of the reproductive justice group SisterReach.
“The same way that we’re knocking on doors and trying to make sure that people vote, we need to be knocking on doors and making sure that people know about the policies that are happening with [religious imposition],” Scott told Rewire.
Scott, Groesbeck, Shepherd, Bertram Roberts, and others are scheduled to appear on a panel Friday evening at Judson Memorial Church in New York City about the new report.
Tell us your story. Have religious restrictions affected your ability to access health care? Email [email protected].
